Jason, a patient of Saeed S. Sadrameli, M.D. arrived at the hospital with excruciating left leg pain and weakness in his foot. Following a minimally invasive endoscopic discectomy to remove a herniated disc, the weakness in his foot was improved, and he went home the very next day.
“He’s really easy to talk to and really down to earth,” shares Jason. “He answered all my questions and even pulled out a little model of the spine so he could tell me what he was going to do. He just made it really easy to sort of understand what was going to happen.”
What is Foot Drop?
 Foot drop, also known as drop foot, is a condition characterized by weakness or paralysis of the muscles that control the movement of the foot and toes, making it difficult to lift the front part of the foot. This can result in dragging the foot while walking and an abnormal gait pattern.
Foot drop, also known as drop foot, is a condition characterized by weakness or paralysis of the muscles that control the movement of the foot and toes, making it difficult to lift the front part of the foot. This can result in dragging the foot while walking and an abnormal gait pattern.
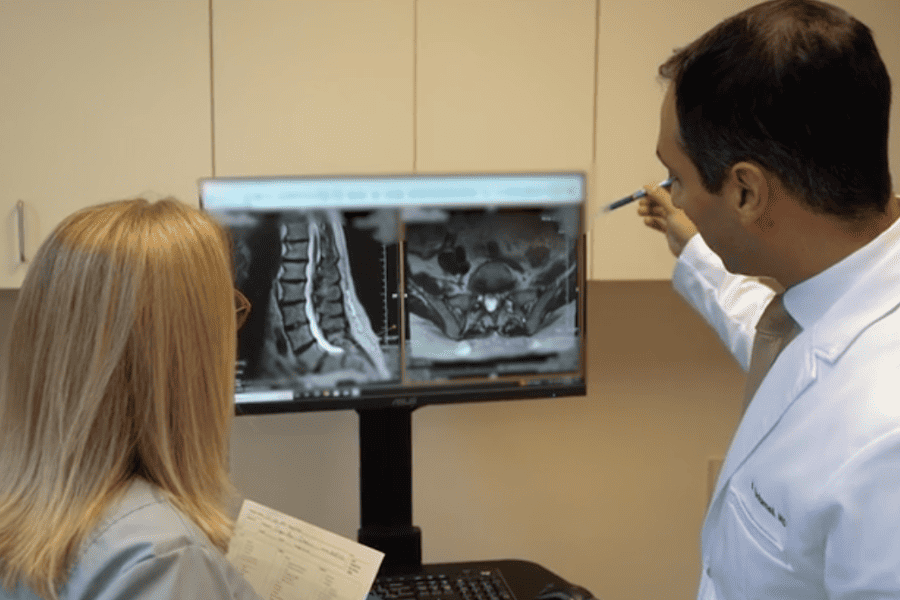
In cases where a herniated disc in the lower spine is causing nerve compression and subsequent foot drop, a neurosurgeon may opt for an endoscopic discectomy. This minimally invasive surgery involves removing the herniated disc through a small incision. This procedure aims to relieve pressure on the affected nerve and restore normal function to the foot.
In Jason’s case, “We were able to use endoscopic techniques through an eight-millimeter incision from the left side of the spine and arrive at the pathology and remove the disc herniation without causing much collateral damage or go through scar tissues from previous surgeries,” says Dr. Sadrameli. ” We saved him from a spinal fusion and he was able to go home the next day, return to his normal activities in 72 hours with significant improvement in his foot weakness.”
What happens during an endoscopic discectomy?
During an ultra-minimally invasive endoscopic discectomy, the surgeon makes an incision the size of a #2 pencil and uses specialized instruments and a thin tube with a camera, known as an endoscope, to access and remove a herniated disc fragment and decompress the nerves in the spine.
Here’s a step-by-step overview of what typically happens during the procedure:
Anesthesia: The patient is usually placed under general anesthesia, ensuring they are asleep and pain-free throughout the surgery. In some cases, awake endoscopic surgery can be offered under local anesthesia with sedation.
Incision: The surgeon makes a small incision, typically 8 millimeters, near the site of the herniated disc. This small incision minimizes tissue damage and blood loss and reduces recovery time and infection rate.
Endoscope insertion: A 7 mm tubular retractor is inserted through the incision to create a path to the affected area. The endoscope, equipped with a camera and light source, is inserted through the tube to provide a clear view of the surgical site displayed on a high definition 4k monitor.
Nerve retraction: The surgeon gently moves aside the nerves and surrounding tissues to access the herniated disc. This step ensures that the nerves are protected during the procedure.
Removal of the herniated disc: Using specialized surgical instruments, such as laser or radiofrequency probe, the surgeon removes the herniated disc and repairs the damaged portion of the disc. This relieves pressure off the spinal nerves and addresses associated pain or other symptoms.
Closure: Once the disc material has been removed, the surgeon carefully removes the endoscope and closes the incision with adhesive glue and covered with a bandaid.
Recovery: After the procedure, the patient is monitored in a recovery area to ensure stability and can typically go home 2 hours after surgery. Patients who undergo endoscopic spine surgery typically do not require narcotics and can return to activities with light duty in 72 hours.
Sign Up for Our Newsletter
Get the latest news and updates from Orlando Neurosurgery delivered straight to your inbox.